The proper diagnosis of a disc herniation in the personal injury patient is an important one. Disc herniations are always abnormal and are usually symptomatic at some point. They also provide the critical link in a personal injury case between injury mechanism and causation of symptoms.
Disc herniations are disc injuries
Disc herniations are abnormal because they represent a disc injury. Disc herniation (or disc failure) is not a result of normal aging. Disc herniations occur in two ways; Repetitive overuse injury or a sudden and dramatic application of force resulting in disc failure.
Repetitive overuse injuries occur when a series of chronic excessive forces are applied to the disc. Each application of force itself is not enough to cause disc failure. However, with successive applications of force, the fibers of the disc annulus (the fibrous band that surrounds the central part of the disc) become stretched, lax and ultimately tear. When disc material enters this tear a herniation occurs. These repetitive overuse injuries are seen in industrial injuries and sports injuries.
A sudden and dramatic application of force is more commonly seen in the personal injury patient. Here, dramatic excessive loads are placed on the disc from falls or automobile accidents. This results in a sudden tearing of the annulus and subsequent herniation.
Disc herniations and pain
A disc herniation may not be painful up to about the first 72 hours after an injury. Disc annulus tears typically occur from the inside of the disc, a region devoid of pain sensing nerves. After several days, the inner disc tear causes sufficient inflammation to activate the nerves of the outer annulus.
Once inflammation sets in after a disc herniation it may not go away. Ultimately, the inflammation associated with a disc herniation may be the cause of most of a patient’s prolonged pain symptoms. In response to the herniation, the body releases inflammatory molecules. This causes more inflammation which brings with it an ingrowth of new nerves into the disc. The entire disc hence becomes sensitized. As a result, a vicious cycle of pain and inflammation sets in. This inflammation can also spread to the epidural space, causing radiculopathy (nerve pain).
Disc herniations also cause symptoms by mass effect. If large enough, there is direct pressure on the spinal sac that carries all the spinal nerves. This is called the dural sac. The dural sac possesses its own nerves and can sense pain. Likewise, there may be mass effect on nerves that have left the dural sac, causing nerve pain.
Disc herniations are focal
By definition, a disc herniation is a focal protuberance beyond the confines of the bone above and below the disc. Spine medical societies have agreed that focal means 25% or less of the disc circumference. If one were to divide the disc into 4 slices of pie, a herniation would occupy one slice of pie or less. If the disc protuberance is bigger than one slice, it is probably a bulge. A bulge implies normal wear and tear, rather than an injury to the disc. However, note that a herniation can occur through a bulge, making diagnosis more difficult.
Types of herniations
Within the classification of a disc herniation, there are several sub-types. When the disc protuberance occupies 25% or less of the disc circumference it is called a protrusion (figure 1).
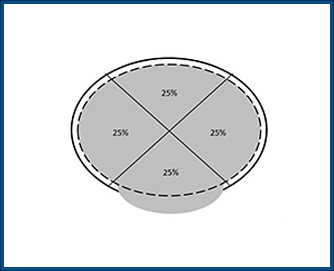
Figure 1
When disc material (shaded) extends beyond its normal margin (dashed line) and the normal vertebra margin (solid line), but involves less than 25% of the disc circumference a herniation is present. This type of herniation is called protrusion.
When the protuberance appears to have squirted out of the disc (when the base or stalk of the herniation is smaller than its widest part) this is called an extrusion (figure 2).
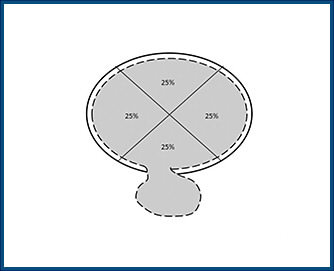
Figure 2
In an extrusion the herniation is attached to the dics by a thin stalk.
When the herniation has disconnected from the disc or stalk this is called a sequestration (figure 3).
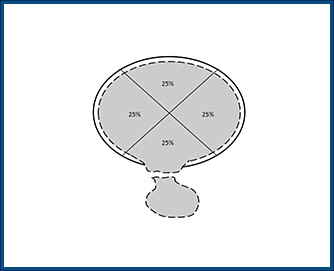
Figure 3
In a sequestration the herniation is disconnected from the disc
Finally, if the herniation has traveled up or down the spine relative to the disc, it’s referred to as a migrated disc herniation (figure 4).
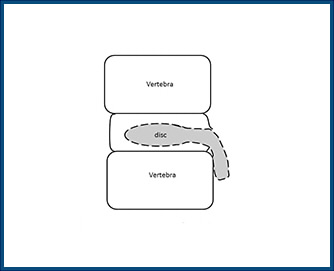
Figure 4
A herniation that travels up or down the spine is referred to as migrated
Some doctors feel that a herniation is not a herniation unless it is an extrusion, a sequestration or has migrated. That is false and excludes from classification the most common type of herniation, the protrusion.
Conclusion
Properly communicating a patient’s condition as a disc herniation is important for plaintiff experts and attorneys trying a case. The disc herniation is abnormal and is caused by injury, therefore it links causation and symptoms. They commonly occur in the PI setting from a sudden and dramatic force which can be supported by experts with biomechanical knowledge, when appropriate. Symptoms can occur sometime after an accident. Symptoms can also occur whether a herniation is big or small. The most common type of herniation is a protrusion. It is distinguished from a bulge by its focality. The common assertion that a herniation is not a herniation unless it is an extrusion or worse is false and excludes the most common type of herniation, a protrusion.
Charles Burton, MD
The views expressed are the personal views of the author and do not represent the views of The Brain, Spine and Joint Group, its managers, affiliates, partners, employees or its clients. Furthermore, the information provided by the author is not intended to be expert or legal advice.
The content of this newsletter is confidential. It is strictly forbidden to copy, forward, reveal the content of or share any part of this newsletter content with any third party, without a written consent of The Brain, Spine and Joint Group. If you received this newsletter, or a link to it, by mistake, please message
